Drive Growth through Digital Credentialing
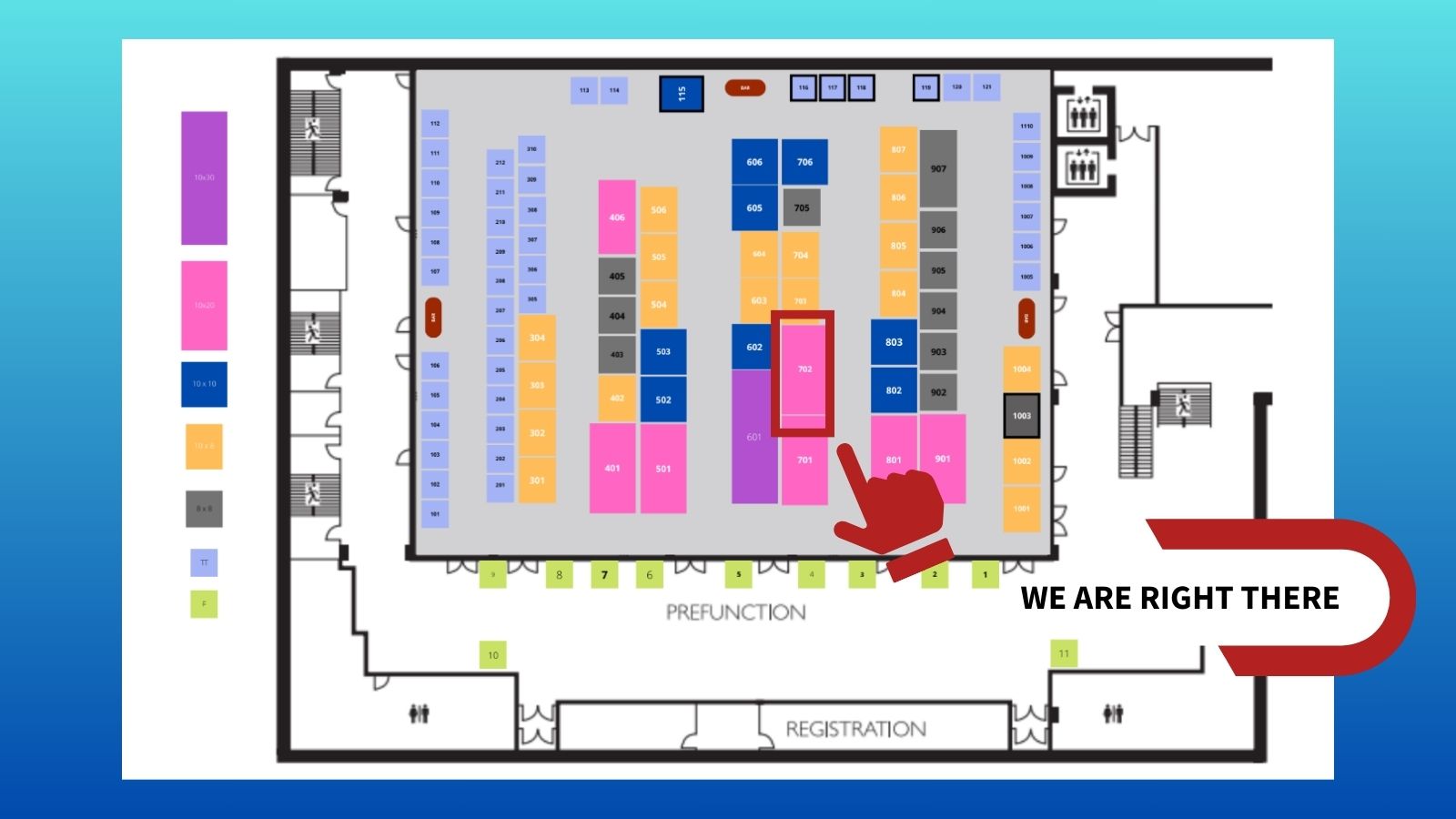
Becker's ASC Conference 2023 Ι October 25 - 28 Ι Swissotel Chicago Ι Booth 702
IntelliCentrics now offers provider credentialing and payer enrollment services on a single, digital platform to reduce administrative costs, accelerate time to care, and ultimately improve patients' access to high-quality care.
Healthcare is facing many operational challenges. We believe using digital technology to streamline the provider credentialing and payer enrollment processes is a low-risk step in creating efficiencies.
We partner with more than 10,000 healthcare facilities to drive compliance and growth through automated credentialing. We have processed 50 million pages of credential documents digitally and support our clients with a full-service team that covers the whole process, from data collection, primary source verification, payer form submissions to expirable management.
Visit us at booth 702 to learn more about our technology and see a demo. Or, use the calendar link below to schedule a meeting with us after the show. 👇
Please complete the form below to request a meeting.
Meet our team

R. Matt Clark
Vice President, Sales

Briana Vona
Regional Vice President, Sales

Adolfo Carrasco
Regional Vice President, Sales
Hear from our customers
“We selected IntelliCentrics because we needed to reduce the average 120-day medical credentialing process to onboard new physicians. Until now, we didn't realize that medical credentialing could generate revenue for us!"
"I have beyond amazing news. We passed the survey without even one corrective action. There was not one flaw in the credentialing files that the auditors went through in great detail. You all have done an amazing job. I have opened 5 facilities, and this is my first facility to have passed surveys without any corrective action. We can’t thank you enough for your hard work."